Vancomycin: Not always effective
Healthcare providers used to freely prescribe Vancomycin to treat infections. This intravenously administered drug is powerful, but stimulated a generation of bacteria that is resistant to its use. Vancomycin is often used to treat organisms that are resistant to other antibiotics. The available treatment options are reduced if resistance develops.
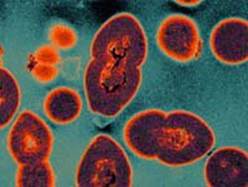
Vancomycin-resistant enterococcus was first detected in 1986. This organism is now prevalent in most hospitals in the United States, where the vancomycin-resistant gene can be transferred to other microorganisms. This can result in spread to many patients. The two species of enterococcus most commonly resistant are E. faecalis and E. faecium (VRFE). Mroe than 39 percent of patients will die after they are infected with VRFE.
VRE causes infections in multiple body sites including the bloodstream, wounds, and urinary tract. Enterococci are normal body flora found in the gastrointestinal tract and are naturally resistant to many antibiotics other than vancomycin. Colonization with VRE, once established, may be indefinite leaving the colonized patient and others at risk of possible infection. Resistant organisms are no more lethal than their non-resistant counterparts, except that they are difficult to treat.
Healthcare providers must control the spread of VRE minimize those at risk. There are four areas of control, which are the standards of care in treating these high-risk patients:
- Prudent and appropriate use of vancomycin (i.e., limit the use of this antibiotic to those circumstances known to be effective).
- Educational programs for staff. These need to be tailored to the specific audience for which intended. For example, physicians need a greater appreciation of the ultimate outcomes of inappropriate prescriptions and use of vancomycin, and to recognize the need to not use this drug in cases of colonization but to “save” it for treatment interventions.
- Infection control measures should be implemented. These include appropriate use of isolation for colonized or infected patients, proper hand decontamination before and after touching patients and contaminated surfaces.
- Detection and reporting of the occurrence of VRE are essential to identify and control the spread. Recognition of the occurrence of VRE allows for proper implementation of control measures including epidemiologic studies to determine those at greatest risk, and measures most effective in minimizing the occurrence of these infections. These may include prompt notification of staff caring for VRE patients.
Modified from “Infections in Hospitals and Nursing Homes” by Ginny Lee, MBA/HCM, MSN, RN, Luke Curtis, MD, MS, CIH, Jacqueline Vance RNC, CDONA/LTC and Lorraine M. Harkavy RN, MS in Patricia Iyer, Barbara Levin, Kathleen Ashton and Victoria Powell, Nursing Malpractice, Fourth Edition 2011
Learn more about how to evaluate liability for urinary tract infections. If a patient gets a urinary tract infection, has someone been negligent? Learn the intriguing answer to this question when you attend the live program to get your questions answered by the speaker, Legal Nurse Consultant Valerie Lane or purchase the digital download to watch at your convenience.