Copy-and-Paste in Medical Records: Prevalence, Risks, and How to Spot It Today
 Electronic health records (EHRs) have revolutionized healthcare documentation, but they come with a copy-and-paste convenience that is a double-edged sword. Copying forward prior notes can save time for busy clinicians, yet overuse of this shortcut (“cloning” documentation) leads to widespread concerns in patient safety, care quality, and legal liability.
Electronic health records (EHRs) have revolutionized healthcare documentation, but they come with a copy-and-paste convenience that is a double-edged sword. Copying forward prior notes can save time for busy clinicians, yet overuse of this shortcut (“cloning” documentation) leads to widespread concerns in patient safety, care quality, and legal liability.
Legal nurse consultants, attorneys, and healthcare professionals must understand how prevalent copy-and-paste documentation is, what risks it poses, and how to recognize it in medical records.
How Common Is Copy-and-Paste in Clinical Documentation?
Ask any LNC who has been reviewing medical records for awhile and you’ll hear stories of copy-and-paste records. Copy-paste use in clinical notes is extremely prevalent in modern practice. Recent studies quantify just how routine this behavior has become:
- Most clinicians use it: Surveys indicate that as many as 90% of clinicians admit to using copy-and-paste functions in the EHR, and 81% acknowledge frequently copying material from another author’s notes urologytimes.com. This is not limited to physicians—nurses, advanced practitioners, and therapists also engage in the practice. Copy-forward features are now standard in major EHR systems, and few providers haven’t at least occasionally used them to save time.
- Half of note content may be cloned: A 2022 analysis of over 100 million EHR notes found that 50.1% of all text in notes was duplicated from prior documentation on the same patient. In 2015, roughly one-third of note text was copied forward; by 2020 that share had swollen to 54.2% ama-assn.org. In other words, more than half of what clinicians read in a patient’s chart might simply repeat older entries. This pattern is present across inpatient and outpatient settings and across all levels of training.
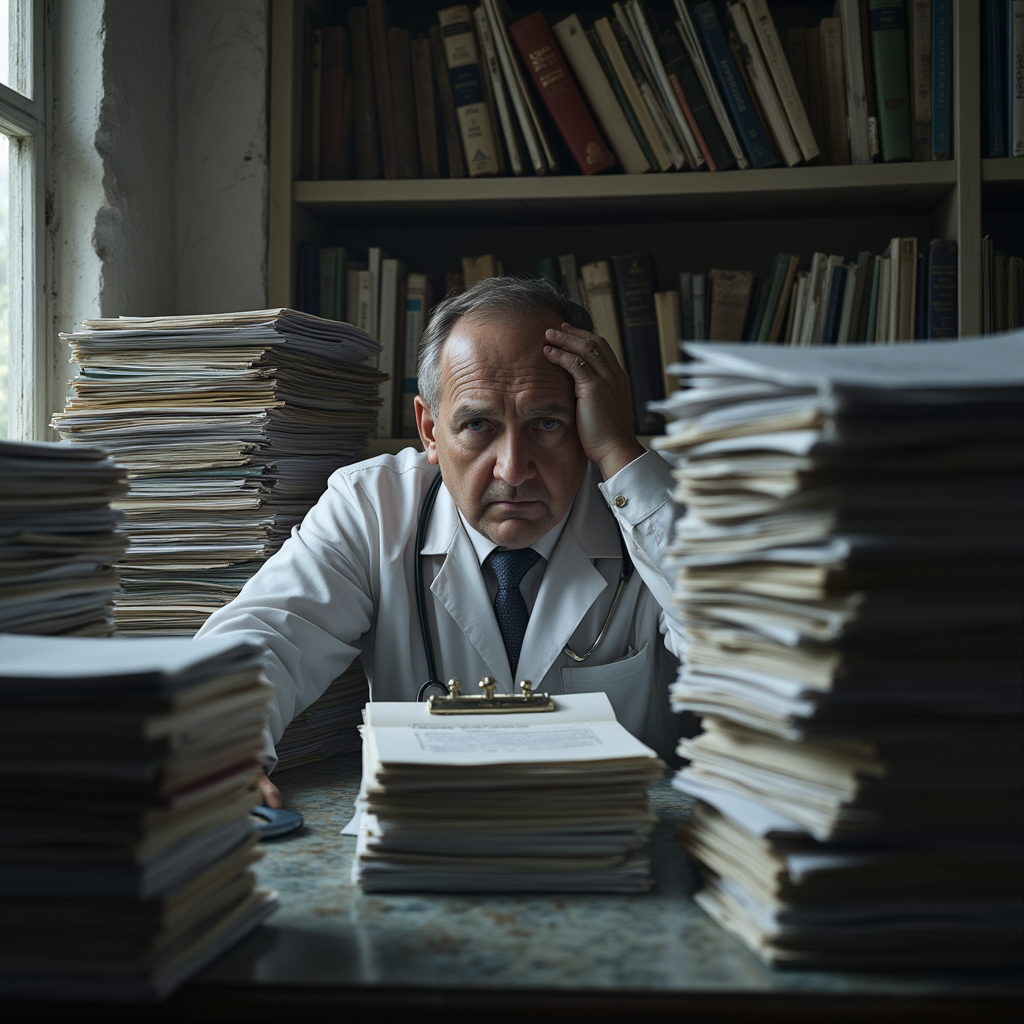
- “Note bloat” is growing: The cumulative effect of cloning is note bloat—ever-lengthening records packed with redundant text. By one estimate, a physician seeing 10 patients in a day might need to sift through 85 pages of documentation (across hundreds of notes) due to duplicated content ama-assn.org. Over time, each additional copied paragraph makes it harder to find new, relevant information. As Dr. Christine Sinsky of the AMA put it, “there is a significant amount of sludge in the system—overdocumentation, too much note bloat to read through,” which contributes to information overload ama-assn.org.
Why do clinicians copy-paste so much? The factors include heavy documentation loads, complex billing requirements, and pressure to save time.
Reusing prior text is seen as a “rational response” to an EHR system not-suited for efficient documentation. As LNCs, we are familiar with sifting through the output of EHRs, with thousands of pages generated by a single admission. There is so much data and often so little information about what we are focused on.
LNCs find that in many hospital medical records, it has become normal for progress notes to be largely copied forward day to day. Despite its benefits for efficiency, this practice has serious downsides that are now well documented.
Copy-and-Paste Risks to Patient Safety, Diagnostic Accuracy, and Care Quality
Copy-paste may streamline workflow, but the patient safety and quality risks are significant. Propagating erroneous or outdated information in a patient’s record can directly harm care. Key dangers include:
- Outdated or wrong information guiding care: When old notes are copied without careful updating, incorrect data can end up in the current record. One EHR study found an egregious example: a patient’s chart contained his wife’s gynecology history, apparently because a physician accidentally copied the spouse’s info into his record and it kept getting carried forward psnet.ahrq.gov. In another case, an abbreviation was misinterpreted – a clinician saw “PE” in the history and assumed it meant pulmonary embolism, when in fact it originally stood for “physical exam”; this copy-paste error led the care team down a diagnostic rabbit hole urologytimes.com. Such propagated errors can result in unnecessary treatments or missed treatments. Incorrect allergies, medications, or histories that persist in cloned notes may cause providers to make decisions on false premises.
- Missed changes in patient condition: If each day’s progress note looks the same as the last, subtle but critical changes can be overlooked. A striking example involved a trauma patient with a spinal epidural hematoma: for five consecutive days, the surgical team’s daily notes repeated “moves all extremities” by copying forward their exam, even as nurses documented emerging paralysis in the legs. The inconsistency went unnoticed. Because the note text wasn’t updated to reflect the patient’s deteriorating neurologic status, a serious complication was missed – resulting in delayed intervention and permanent paralysis psnet.ahrq.gov. As we know as LNCs, over-reliance on autopopulated exam findings can directly jeopardize diagnostic accuracy and patient safety.
- Internal inconsistencies and confusion: A cloned note can contain contradictions that make the medical record incoherent. For instance, I have found medical records with an entry that listed a procedure or surgery as scheduled for “tomorrow” even though it was already done yesterday – a clear sign that yesterday’s note was copied forward without updating. Notes may reference symptoms that the patient no longer has (or never had) because the author failed to remove outdated information. These inconsistencies confuse anyone reading the chart and undermine trust in the documentation. They also impair care coordination: when multiple providers (physicians, nurses, consultants) all copy from one another, errors or omissions spread virally through the record. In a complex case with many team members, this can mean no one has an accurate picture of the patient’s status. And we know that can lead to misdiagnosis, delayed diagnosis, and improper treatment.
- Note bloat and information overload: Quantity can obscure quality. Bloated notes filled with duplicative text make it harder for clinicians to find important new information ama-assn.org. Critical updates (a new test result, a changed medication) may be buried in pages of pasted material goldsmithlegal.com. Time-pressed providers might skim over the redundancy or skip reading notes altogether, increasing the risk of oversight. As one study noted, the duplicated half of note content “provides no new information, but increases the time required for the reading clinician to discern what is accurate and timely vs. false or irrelevant” ama-assn.org. In short, copy-paste can turn the medical record into a cluttered data dump, where finding the needle of truth in the haystack is difficult. Our role as LNCs is often to find the needle of truth, and we have the luxury of time to do that analysis, compared to the clinicians who need to comb through medical records for the significant and current data about the patient.
- Delayed or missed diagnoses: Copy-paste practices have been linked to diagnostic errors. A review by the Partnership for Health IT Patient Safety found that in one study, 2.6% of diagnostic errors requiring additional care were attributable to copy-paste issues digitalassets.jointcommission.org. An example is the “denies fever” problem: A clinician might paste a prior note’s phrase “Patient denies fever, chills, cough” into today’s history without verifying, causing them to downplay a new low-grade fever that is actually an early sign of infection. Important clues can be lost in a copied narrative, delaying recognition of serious conditions like sepsis goldsmithlegal.com. In a safety report on a fatal missed diagnosis, a primary care physician had copied the same assessment and plan for two years’ worth of visits – thereby failing to follow up on a recommended cardiac stress test. The patient later died of a heart attack, and the investigation found that the physician’s copy-forward habit contributed to the missed diagnosis digitalassets.jointcommission.org.
- Provider burnout and communication breakdown: From a human factors standpoint, bloated documentation contributes to clinician burnout and impedes effective communication. Physicians already spend hours on EHR data entry and review; reading through reams of redundant text only adds to the burden ama-assn.org. Studies have associated excessive documentation (including copy-paste) with wasted time and increased likelihood of errors and burnout ama-assn.org. Furthermore, when notes are not trustworthy or readable, the medical team’s communication suffers. Nurses might not rely on physician notes if they suspect they’re just templated repeats, and vice versa psnet.ahrq.gov. Accurate, succinct notes are essential for high-quality care. Copy-paste short-cuts can sabotage that clarity.
 In summary, while copy-paste can improve efficiency, it is not a benign user practice. It can lead to note inaccuracies, patient harm, and a breakdown in documentation quality that ultimately affects patient outcomes.
In summary, while copy-paste can improve efficiency, it is not a benign user practice. It can lead to note inaccuracies, patient harm, and a breakdown in documentation quality that ultimately affects patient outcomes.
Dig deeper into medical records with our free report, which will give you practical tips. Get our free report, 9 Secrets of Analyzing Medical Records.
Get these tips in our free report on analyzing medical records at this link.
Get your copy of Medical Record Analysis Vol 4. Go here
 Pat Iyer is president of The Pat Iyer Group, which develops resources to assist LNCs in obtaining more clients, making more money, and achieving their business goals and dreams.
Pat Iyer is president of The Pat Iyer Group, which develops resources to assist LNCs in obtaining more clients, making more money, and achieving their business goals and dreams.
Have you heard the most recent podcasts on Legal Nurse Podcast? The show is in its 9th year, putting it in the top 1% of all podcasts for its longevity. Watch our podcast on YouTube at http://LNC.tips/YouTube.
Join our Facebook group, LNC Business Growth Circle, to be part of our LNC community.
Pat’s related websites include the podcasts broadcast at podcast.legalnursebusiness.com, and writing tips supplied at patiyer.com.
Get all of Pat’s content in one place by downloading the mobile app, Expert Edu at www.legalnursebusiness.com/expertedu. Watch videos, listen to podcasts, read blogs, watch online courses and training, and more.
